Social Health Protection
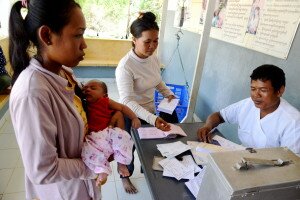
Making free public healthcare attractive: optimizing Health Equity Funds in Cambodia
Health Equity Funds (HEF) were developed to enable poor people access to public health services by paying public health providers on their behalf, including non-medical costs for hospitalised beneficiaries (HEFB). The national scheme covers 3.1 million pre-identified HEFB. Uptake of benefits, however, has been mixed and a substantial proportion of poor people still initiate care at private facilities where they incur considerable out-of-pocket costs. We examined the benefits of additional interventions compared to existing stand-alone HEF scenarios in stimulating care seeking at public health facilities among eligible poor people.
We report on three configurations of HEF and their ability to attract HEFB to initiate care at public health facilities and their degree of financial risk protection: HEF covering only hospital services (HoHEF), HEF covering health centre and hospital services (CHEF), and Integrated Social Health Protection Scheme (iSHPS) that allowed non-HEFB community members to enrol in HEF. The iSHPS also used vouchers for selected health services, pay-for-performance for quantity and quality of care, and interventions aimed at increasing health providers’ degree of accountability. A cross sectional survey collected information from 1,636 matched HEFB households in two health districts with iSHPS and two other health districts without iSHPS.
Compared to other HEF arrangements, iSHPS saw 56% of HEFB initiate care seeking at public health facilities, much more than 13-40% at control sites. Inclusion of health centres in HEF arrangements appears instrumental to improve care seeking at all levels of public health facilities by HEFB. The overall costs associated with care seeking at iSHPS sites was US$10.4, which was 87% to 99% lower than control sites. Driving factors for these lower costs in comparison with control sites appeared to be the high use of primary health care facilities, lower user fees at public health facilities as well as at private facilities, and reduced tendency to seek care at non-medical providers.
More: Making free public healthcare attractive: optimizing health equity funds in Cambodia
Attracting poor people to public health facilities to access free health care: an assessment of the Integrated Social Health Protection Scheme
Cambodia introduced user fees in the public health sector in the late 1990s whereby utilisation of public sector health services increased although the poor saw their financial access decreased. To safeguard the positive effects of user fees on staff performance while ensuring access to health care for the poor, Health Equity Funds (HEF) were established and their coverage has expanded over time. A substantial proportion of HEF beneficiaries (HEFB) still initiate healthcare seeking at private health providers where they incur considerable expenses. Here we report on the effects of three HEF configurations on financial access to public health facilities by HEF beneficiaries: [1] Integrated Social Health Protection Scheme (iSHPS) that also employed vouchers for selected health services, pay-for-performance and interventions aimed at improving health systems governance structures and quality of health services; [2] Standard HEF where HEF coverage is only available at a hospital; and [3] Comprehensive HEF where HEF coverage is available at both health centre level and hospital level.
Data were collected from four operational districts (OD): 2 ODs as intervention areas and 2 control ODs where the HEF scheme had been implemented without participation in the pilot iSHPS. Study respondents were men and women aged 18-59 years and included 767 respondents from iSHPS areas and 869 respondents from control ODs.
Compared to other HEF arrangements, iSHPS saw 56% of HEFB initiate care seeking at public health facilities, much more than 13-40% at control sites. The overall costs associated with care seeking at iSHPS sites was US$10.30; 81% to 101% lower than such costs observed at control sites. Driving factors for these lower costs in comparison with control sites appeared the high use of primary health care facilities, lower user fees at public health facilities as well as at private facilities, and reduced tendency to seek care at non-medical providers.
Report:
Working paper on Attracting poor people to public health facilities to access free health care
Financial access to health care for older people in Cambodia: 10-year trends (2004-14) and determinants of catastrophic health expenses
Older people make up an increasing proportion of the population in low- and middle-income countries. This brings a number of challenges, as their health requirements are greater than, and different from, those of younger people. In general, these health systems are not geared to address their needs, and traditional support systems tend to erode, potentially causing financial hardship when accessing health care. This paper provides an overview of older Cambodians’ financial access to health care over time, using nationally representative data to enable the formulation of appropriate responses.
Link: http://www.equityhealthj.com/content/pdf/s12939-016-0383-z.pdf
Access to Health Care and Associated Out-of-pocket Expenditures for People with Disabilities, People with Chronic Diseases and Older People in Cambodia (2016)
Over the last 30 years Cambodia has experienced a dramatic demographic and economic shift, propelling it from one of the poorest countries in the world to lower middle-income status in a single generation. Life expectancy is quickly increasing, and the proportion of people aged 60 or older is expected to rise to over 20% of the population in 2060. This shift brings new challenges in health care; while communicable diseases remain a serious concern, non-communicable chronic conditions are becoming more prominent while others such as disabilities remain serious concerns. This transition presents new issues for the Royal Government of Cambodia and its health partners in providing all citizens with access to quality health services. However, there is a considerable overlap between older people, those with disabilities and those with chronic diseases, suggesting that similar mitigation strategies may be effective for these groups.
This report presents the findings of a secondary analysis of data from the Cambodian Socio-Economic Surveys in 2004, 2007 and annual data from 2009 to 2013. This data was examined to understand the trends in financial access to health care and treatment of households with older people, those with disabilities, and those with chronic diseases. Additional regression models were constructed to analyse the determinants of key variables, especially out-of-pocket and catastrophic expenditures, and impoverishment due to health care costs.
The findings show that these three vulnerable groups are more prone to illnesses and access health care more frequently than other groups. Their access to health care has improved dramatically since 2004, but they pay considerably more for this care than other individuals, and are thus more likely to face catastrophic health expenditures, impoverishment and indebtedness through illness.
Report:
From Health Equity Funds to Integrated Social Health Protection Schemes: Evidence from Kampot and Kampong Thom Operational Health Districts from 2010-2012
Since 2008, the Cambodian-German Social Health Protection Programme has promoted the extension of health equity funds (HEFs) into integrated social health protection schemes (ISHPSs). Vulnerable households, such as the near-poor and those at risk of high health expenditures, can enrol voluntarily in the schemes through affordable contributions. This transitional strategy toward universal health coverage targets public subsidies to the families that demand public health services and still empowers them as clients.
In 2012, ISHPSs covered all health centres and referral hospitals in Kampong Thom and Kampot Operational Health Districts (ODs). Approximately 30% of the population in Kampong Thom and 16% in Kampot OD were covered by the schemes. The majority of members were classified as poor and exempted from any contribution. The utilisation rates of members were well above the national average. This suggests that the schemes were successful in improving equity and efficiency of public services through increased utilisation among the poor and vulnerable.
Additional benefits, such as transport vouchers, were shown to be an effective way to increase utilisation of health services by poor members. Faith-based organisations mobilised community resources to finance transport vouchers, and ensured the engagement of local religious and community leaders for promotional and outreach activities, hereby building trust of the community. Safe motherhood grants increased the proportion of institutional deliveries as well as compliance with pregnancy and newborn check-ups.
Report:
From Health Equity Funds to Integrated Social Health Protection Schemes
Assessing operational efficiency of the integrated social health protection schemes of Kampong Thom province (2014)
As a transitional approach towards universal health coverage, Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) GmbH has supported the piloting of integrated social health protection schemes (ISHPS) in Kampong Thom province. These schemes aim to improve access to public health services for the poor and vulnerable, and increase the utilisation and efficiency of these services. ISHPS is built on the well-established health equity fund (HEF) system, which targets the poorest households with free public health care, as well as transportation and food allowances in the event of hospitalisation. ISHPS extends the scope of HEFs by enabling vulnerable households to access health care by enrolling in the existing scheme for a symbolic contribution. The scheme promotes accountability
the piloting of integrated social health protection schemes (ISHPS) in Kampong Thom province. These schemes aim to improve access to public health services for the poor and vulnerable, and increase the utilisation and efficiency of these services. ISHPS is built on the well-established health equity fund (HEF) system, which targets the poorest households with free public health care, as well as transportation and food allowances in the event of hospitalisation. ISHPS extends the scope of HEFs by enabling vulnerable households to access health care by enrolling in the existing scheme for a symbolic contribution. The scheme promotes accountability and quality improvement by using a pay-for-performance mechanism for affiliated
and quality improvement by using a pay-for-performance mechanism for affiliated health centres. It is strengthened by a voucher programme, also financed by the German Government, which in addition aims to increase demand for specific priority services.
health centres. It is strengthened by a voucher programme, also financed by the German Government, which in addition aims to increase demand for specific priority services.
As part of the 2013 ISHPS baseline evaluation in Kampong Thom province, GIZ commissioned to the Population Council an organisational assessment of the ISHPS in the Kampong Thom and Stong operational health districts. The objective of the assessment was to improve the efficiency and effectiveness of ISHPS. This report discusses the potential efficiency gains to be found in the core functions of the scheme: stewardship, revenue collection, pooling and purchasing mechanisms.
Report:
Out-of-Pocket and Catastrophic Expenditure on Health in Cambodia (2011)
Cambodian Demographic Health Survey 2005 and
Socio-Economic Surveys 2004 & 2007 Analysis
 Seeking health care when needed without financial burden is at the heart of the principles embodied by the concept of universal health coverage. However, to make this concept a reality, countries have to undertake a reform of their social health protection policies. Such reforms need to be informed by reliable evidence on the needs of populations and vulnerable groups.
Seeking health care when needed without financial burden is at the heart of the principles embodied by the concept of universal health coverage. However, to make this concept a reality, countries have to undertake a reform of their social health protection policies. Such reforms need to be informed by reliable evidence on the needs of populations and vulnerable groups.
The present report looks at key indicators of the financial burden and associated health-seeking behaviour of various socioeconomic groups in Cambodia before the implementation of the Second Cambodian Health Strategic Plan (HSP2) in 2008. Using data from the previous Cambodian Socio-Economic Surveys (CSES) in 2004 and 2007, and the Cambodian Demographic Health Survey (CDHS) 2005, it illustrates the challenge that the Royal Government of Cambodia faced with its health partners in reducing out-of-pocket health expenditures and providing all its citizens with access to quality health services.
The analysis used robust and internationally recognised methods to quantify catastrophic expenditures and impoverishment resulting from seeking health care. It also examined the determinants of these indicators, and discussed the associated policy implications.
The CDHS 2005 analysis shows the need for increased health care access among the poorest groups of the population, as well as for old people, women and children under 5 years old. It confirms the important role of private providers in the delivery of services, but also in the financial landscape, with the great majority of health care visits and expenditures channelled to the private sector. Direct costs related to seeking care, such as transportation, were also significant, representing on average over 10% of household spending on health.
The CSES analysis provides a similar picture, but also illustrates how catastrophic expenditures, debt and impoverishment from health care are a risk for all economic groups, particularly those in rural areas or as a result of hospitalisation of a family member.
The vision of the Royal Government of Cambodia and the Ministry of Health to progress towards universal health coverage is shared by the Federal Republic of Germany, which provides technical support in this endeavour through the Cambodian-German Social Health Protection Project implemented by Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ).
in this endeavour through the Cambodian-German Social Health Protection Project implemented by Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ).
Report:
Cambodian Demographic Health Survey 2005 and Socio-Economic Surveys 2004 & 2007 Analysis - khmer
Cambodian Demographic Health Survey 2005 and Socio-Economic Surveys 2004 & 2007 Analysis - english
Out-of-Pocket and Catastrophic Expenditure on Health in Cambodia (2012)
Cambodian Socio-Economic Surveys 2004, 2007 & 2009 Analysis
 Information on health care costs, such as the burden of out-of-pocket household health spending and the extent of catastrophic health expenditures is essential for monitoring programmes, but also for guiding interventions, creating policy dialogue, and instituting reforms to achieve universal health coverage. Using robust and recognised methodologies, the following report presents a quantitative analysis of such indicators.
Information on health care costs, such as the burden of out-of-pocket household health spending and the extent of catastrophic health expenditures is essential for monitoring programmes, but also for guiding interventions, creating policy dialogue, and instituting reforms to achieve universal health coverage. Using robust and recognised methodologies, the following report presents a quantitative analysis of such indicators.
It uses a secondary statistical analysis of data from the Cambodian Socio-Economic Surveys (CSES) in 2004, 2007 and 2009 to illustrate the positive trend in access to health services, especially for the poor over that time. The analysis also points to the added value of the strategic interventions delineated by the Second Cambodian Health Strategic Plan (HSP2) for the years 2008-2015, and raises policy implications for further developing social health protection mechanisms for all Cambodians.
Between 2004 and 2009, all economic population groups reported a significant improvement of their health status, and more people sought medical care when sick. At the same time, overall out-of-pocket expenditures on health care rose significantly from KHR 59,640 to KHR 117,852 per person annually. However, average heath care bills also more than doubled. This rapid inflation was counterbalanced by increases in income during the same period. As a result, there was a significant decrease in catastrophic health expenditures, from 6.02% to 4.27% of all households spending more than 40% of their capacity-to-pay on health. This positive result is also partially explained by the government’s efforts to extend social health protection to the poorest people. However, the risk of impoverishment and indebtedness from high health care costs remains a reality for almost all Cambodians, particularly for old people and people in need of hospital care. These results underline the importance of advancing the agenda for universal health coverage in Cambodia as a way to foster economic, social and human development.
The vision of the Royal Government of Cambodia and the Ministry of Health to progress towards universal health coverage is shared by the Federal Republic of Germany, which provides technical support in this endeavour through the Cambodian-German Social Health Protection Project implemented by Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ).
Report:
Cambodian Socio-Economic Surveys 2004, 2007 & 2009 Analysis – khmer
Cambodian Socio-Economic Surveys 2004, 2007 & 2009 Analysis – english
Social Health Protection Activities in Kampot, Cambodia – 2009 Baseline
From 2007 to 2012, GIZ supported the development and implementation of a social health protection scheme in Kampot province in collaboration with the Groupe de Recherche et d’Echanges Technologiques (GRET). The project provided fully subsidised health care coverage for poor households to access public health facilities, as well as reimbursements for non-medical costs such as transportation and food for inpatient services. Voluntary enrolment in the scheme was also available for vulnerable and near-poor households through prepaid contributions. The following report provides an overview of the 20 health indicators developed to evaluate the scheme’s impacts as of 2009.
the development and implementation of a social health protection scheme in Kampot province in collaboration with the Groupe de Recherche et d’Echanges Technologiques (GRET). The project provided fully subsidised health care coverage for poor households to access public health facilities, as well as reimbursements for non-medical costs such as transportation and food for inpatient services. Voluntary enrolment in the scheme was also available for vulnerable and near-poor households through prepaid contributions. The following report provides an overview of the 20 health indicators developed to evaluate the scheme’s impacts as of 2009.
Scheme members in Kampot OD, including the very poor, were more likely to utilise public health services for health shocks than non-members and better-off households. Children under five years old and the very poor had 80% and 50% higher odds of ever using a health centre than individuals in other age groups and households in different wealth categories. Scheme members also sought treatment an average of 1.2 days earlier than non-members. The very poor delayed treatment longer than other groups studied (an average of 8.3 days after the start of the incident).
The impact of health shocks was considerable; the average patient lost 28 days of normal activity per incident, with caregivers losing an additional 18 days. Scheme members lost less days than non-members. About one in five households surveyed (22.6%) had health-related debt. Scheme members had less health-related debt than non-members, both in terms of real value, and expressed as a proportion of all household debt (23.1% and 27.9%, respectively).
Report:
Social Health Protection Activities in Kampot, Cambodia – 2009 Baseline
Impact of an Integrated Social Health Protection Scheme in Kampot, Cambodia – 2008 to 2010
From 2007 to 2012, GIZ supported the development and implementation of a social health protection scheme in Kampot province through the Groupe de Recherche et d’Echanges Technologiques (GRET). The project provided fully subsidised health care coverage for poor households to access public health facilities, as well as reimbursements for non-medical costs such as transportation and food for inpatient services. Voluntary enrolment in the scheme was also available for vulnerable and near-poor households through prepaid contributions. The following report provides an examination of the impact of the scheme on voluntary members in Kampot operational health district (OD) from 2008 until 2010.
Report:
Impact of an Integrated Social Health Protection Scheme in Kampot, Cambodia – 2008 to 2010
Actuarial Review of The NSSF Employment Injury Branch and Assessment of Social Health Insurance
for The National Social Security Fund (NSSF) and The National Social Security Fund for Civil Servants (NSSFC)
Report:
Actuarial Review of the NSSF Employment Injury Branch and Assessment of Social Health Insurance
Determinants of Non-Utilisation of Public Health Services among Poor Households Covered by a Social Health Protection Scheme
An Evaluation in Kampot Operational District, Cambodia
Report:
Working Papers and Policy Briefs
Briefings for Health Financing Policy-Making in Cambodia
This series of policy briefs intends to support and inform decision-makers in Cambodia on key issues related to health financing and social health protection. These briefs are not scientific papers, but rather summarise evidence and technical concepts that decision-makers may consider in their discussions. – All briefs are available in Khmer and English.
Briefing #1 – Extending Social Health Protection in Cambodia: How can health equity funds pave the way for universal health coverage?
Out-of-pocket expenditures on health are a major challenge for Cambodia’s population; they cause indebtedness and impoverishment across all population groups, and pose considerable barriers to accessing health care, especially for poor and vulnerable groups such as old people, people with disabilities, the near-poor and people with unreliable work. To address these challenges, Cambodia’s current draft health financing policy foresees the development of social health protection (SHP) schemes targeting different segments of the population. Currently, health equity funds (HEFs) are the most widespread SHP scheme in Cambodia.
HEFs target the poorest segment of the population. However, differences in income between the poor and the majority of the population are small, especially in rural areas. Households not meeting the strict national poverty criteria are excluded from HEF benefits even if specific risk factors, such as chronic disease, would justify their inclusion. In addition, HEF schemes face a major challenge as the costs per beneficiary rise. This is due to smaller pools of potential beneficiaries, resulting from decreasing poverty and higher benefit reimbursement rates. Extending the role of HEF schemes beyond their current focus on the poorest members of society would address those concerns.
Briefing #2 – Transitioning from Voluntary Micro Insurance to Universal Health Coverage: Could Cambodia follow Ghana’s path?Cambodia’s current draft health financing policy foresees the development of financing schemes targeting different segments of the population, with the ultimate goal of transitioning to a unified system to achieve universal health coverage. A key element in this policy is reducing the fragmentation of existing social health protection (SHP) schemes.These policy endeavours could benefit from the experience of other developing countries, especially Ghana – a low-income country in sub-Saharan Africa that faced similar challenges a decade earlier. In 2003 Ghana established its National Health Insurance Scheme (NHIS). With NHIS, Ghana consolidated the different community-based health insurance (CBHI) schemes in the country into a single national programme by enacting key legislation and structural reforms.
Briefings:
Transitioning from Voluntary Micro Insurance to Universal Health Coverage-khmer
Transitioning from Voluntary Micro Insurance to Universal Health Coverage-english
Briefing #3 – Access to Public Health Services: Why do eligible households not make use of health equity fund benefits?
The costs associated with using health services pose a major challenge for Cambodia’s poor. This led to the emergence of a number of social health protection (SHP) schemes targeting poor households, the most widespread being health equity funds (HEFs). HEFs cover both poor households’ health care costs at public facilities and direct non-medical costs such as transportation and food (for hospital inpatients and caretakers). The geographic expansion of HEF schemes is a significant development towards universal health coverage (UHC). Nevertheless, careful analysis of utilisation data among HEF beneficiaries raises questions about the extent to which beneficiaries actually make use of the scheme in case of sickness.
Briefings:
Access to Public Health Services-khmer
Access to Public Health Services-english
Briefing #4 – The Transition to Universal Health Coverage in Cambodia: It is about the poor… but not only.
The Royal Government of Cambodia is aware of the challenges that direct and indirect health care costs represent for the population, and has supported and begun a number of social health protection (SHP) initiatives targeting different segments of the population, while working towards the ultimate goal of universal health coverage(UHC). The largest and most studied of these initiatives are health equity funds (HEFs). Cambodia has also initiated the establishment of social health insurance funds for workers in the formal sector, which are expected to begin in 2015. However, most of the population remains in the informal economy and is progressively moving out of poverty to a precarious ‘near-poor’ status. This group remains very vulnerable to economic shocks, which can push them back into poverty or hinder their economic progress through lost income or long-term debt.
In this briefing note, we look at the financial burden that health care puts on Cambodian families and the determinants (explanatory factors) that contribute to, or protect them from, catastrophic health spending. We conducted our analysis using the latest large-scale consumption surveys for which in country data is available – the 2004 and 2009 Cambodian socio-economic surveys (CSES). The evidence presented should guide decision-makers in setting priorities and policies in the transition to UHC.
Briefings:
The Transition to Universal Health Coverage in Cambodia-khmer
The Transition to Universal Health Coverage in Cambodia-English
Briefing # 5: Mental Wellbeing among the Poor: Do health equity funds protect them from stress and financial hardship?
Catastrophic spending and indebtedness due to health care needs are significant challenges for households in Cambodia. Health equity funds (HEFs) and strategies such as the Integrated Social Health Protection Scheme (ISHPS)[1] have been designed to enable affordable access to health care at public facilities for poor and vulnerable households, and prevent health-related financial hardship. But HEF schemes tend to be underutilised, and large numbers of eligible households still make out-of-pocket (OOP) payments for health care. The majority of these households resorts to borrowing to pay for these costs. Cambodians’ heavy reliance on private health care is partly responsible for this.
When borrowing for health care, the poor typically utilise informal moneylenders with exorbitant interest rates. The poorest Cambodians can incur average annualised interest rates of 170% when borrowing money for health care. Such high rates put an extreme amount of stress on people and may affect their overall health; debt is a predictor of increased stress, depression, and worse general health status. The interaction between health care indebtedness and health status in Cambodia has received little attention to date, whereby this briefing note presents some of the latest evidence on this issue from four operational health districts (ODs) covered by social health protection schemes.
[1] See “Briefings for Health Financing Policy-Making in Cambodia – #1. Extending Social Health Protection in Cambodia: How can health equity funds pave the way for universal health coverage?”
Briefings:
Mental Wellbeing among the Poor – Mental health and lending-Khmer
Mental Wellbeing among the Poor – Mental health and lending-English
Briefing #6: Cervical Cancer in Cambodia: Can we afford not to address it?
Non-communicable diseases (NCDs) are on the rise, worldwide and in Cambodia, with an immense negative impact on societies and health systems. NCDs threaten to exacerbate poverty and exert an enormous cost on the Cambodian economy. The World Health Organization estimates that the four most severe NCDs (cardiovascular diseases, cancer, chronic respiratory diseases and diabetes) cause about 50% of all deaths in Cambodia, and this figure is projected to rise further as a consequence of changes in lifestyle and environment. Fighting NCDs requires a mix of interventions, combining preventive and therapeutic strategies. Implementing such a disease-based approach is a complex endeavour and demands a well-structured health system.
This paper gives an overview of the disease burden of cervical cancer in Cambodia, and the rationale for preventive and therapeutic actions against it, arguing that such actions can be cost-effective, as also technically and financially feasible.
Briefings:
Cervical Cancer in Cambodia-Khmer
Cervical Cancer in Cambodia-English
Working papers
Working paper #1 – Toward universal health coverage: the Cambodian experience formulating a health financing policy
Universal health coverage is high on the international policy agenda, and appears set to become the post-2015 overarching sustainable development goal. Achieving universal coverage is by no means an easy undertaking that can be attained in a relatively short time period, and as such requires a roadmap. Despite its relevance, surprisingly little has been written about the process of developing and formulating a health financing policy.
In Cambodia, the Ministry of Health has stated the processes and interventions it intends to use to achieve universal health coverage in a health financing policy. This essay provides an overview of the Cambodian health financing policy formulation process, by applying a modified analytical framework that covers priority setting, policy option formulation and appraisal, and policy finalisation. Formulation of policy options was steered by the policy’s vision as well as its guiding principles. In addition, this process was informed by a comprehensive situation analysis. Policy formulation happened in a relative short time period, and involved extensive stakeholder consultations for general guidance in tandem with teasing out more detailed options by a core group of technical people.
Processes related to the endorsement or rejection of the policy by upper legislative bodies are not discussed, although caution was applied to consider political actors’ viewpoints during formulation. This should facilitate positive receipt of the document by them.
Working paper:
Toward universal health coverage: the Cambodian experience formulating a health financing policy
WORKING PAPER – Costing of Type 2 Diabetes Mellitus in Cambodia: Micro-costing, budget-impact and cost-effectiveness analysis
Type 2 diabetes mellitus (T2DM) is a major and growing medical, social and economic burden for Cambodia. This paper forecasts the epidemiological and economic consequences of T2DM and discusses the most cost-effective interventions against T2DM.
T2DM is a major public health challenge in Cambodia, but the economic simulations clearly indicate that prevention and treatment of this disease is highly cost-effective. However, not all interventions that are cost-effective are also feasible, given limited resources.
The introduction of a combined screening programme and full coverage of all patients requiring OAD or insulin therapy would result in nearly 600,000 years of life saved and 78,000 death cases averted within the simulation period. The number of diagnosed diabetic cases would increase from around one-third of all diabetes patients (37%) to nearly all (89%). Among diagnosed patients, the number with complications would decline from 68% to 51%. More patients would not require any medication (9% instead of 8%), but also more patients would require insulin (21% instead of 17%). Assuming implementation of this combined intervention in 2008, the annual budget for professional diabetes prevention and treatment that year would have been nearly USD 8 million.
Working paper:
WORKING PAPER: Costing of Cervix Uteri Carcinoma in Cambodia: Budget-impact and cost-effectiveness analysis
Cervix uteri carcinoma (CUC) is a malignant neoplasm that is almost exclusively caused by a persistent infection of the human papilloma virus (HPV). This disease is the second most common cancer in women worldwide, with around 500,000 new cases and 270,000 death cases annually. In Cambodia, it is estimated that around 800 death cases per year are caused by CUC. The number of deaths due to cervical cancer has grown faster than the population. Each year, around 5,000 years of life are lost due to CUC.
Combining treatment, screening and vaccination scenarios has a greater impact on the number of death cases than individual interventions, but the budget required to implement combined interventions is also much higher. Based on the results of the model presented in this paper, the ‘see-and-treat’ approach combined with a vaccination programme would be most cost-effective.
The results of the simulations in this paper indicate that there are cost-effective interventions to prevent and treat CUC that could be financed with limited budgets. Based on these simulations, the Royal Government of Cambodia should include a ‘see-and-treat’ approach to CUC care in the basic package of health care services, and begin a HPV vaccination programme as soon as possible.
Working paper:
Costing of Cervix Uteri Carcinoma in Cambodia: Budget-impact and cost-effectiveness analysis

